PRACTICAL OF ABO AND Rh TYPING
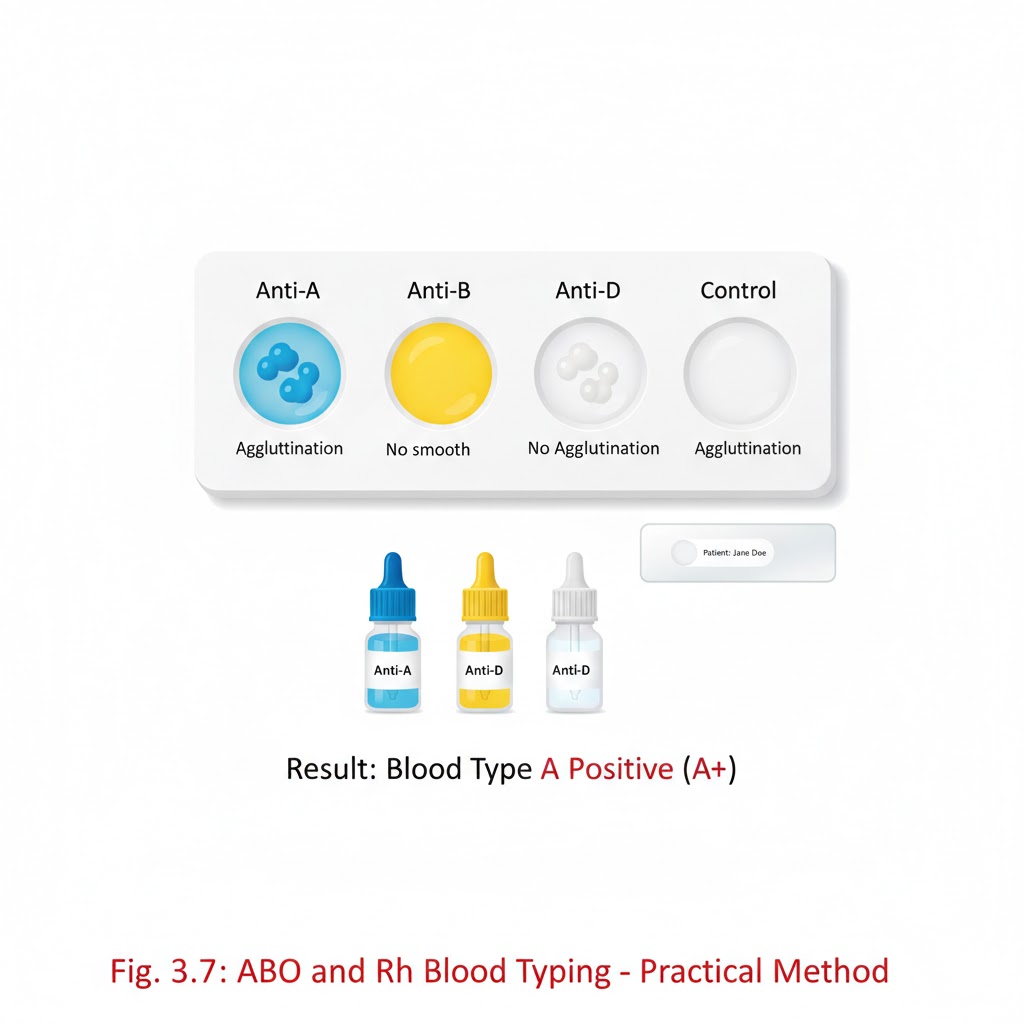
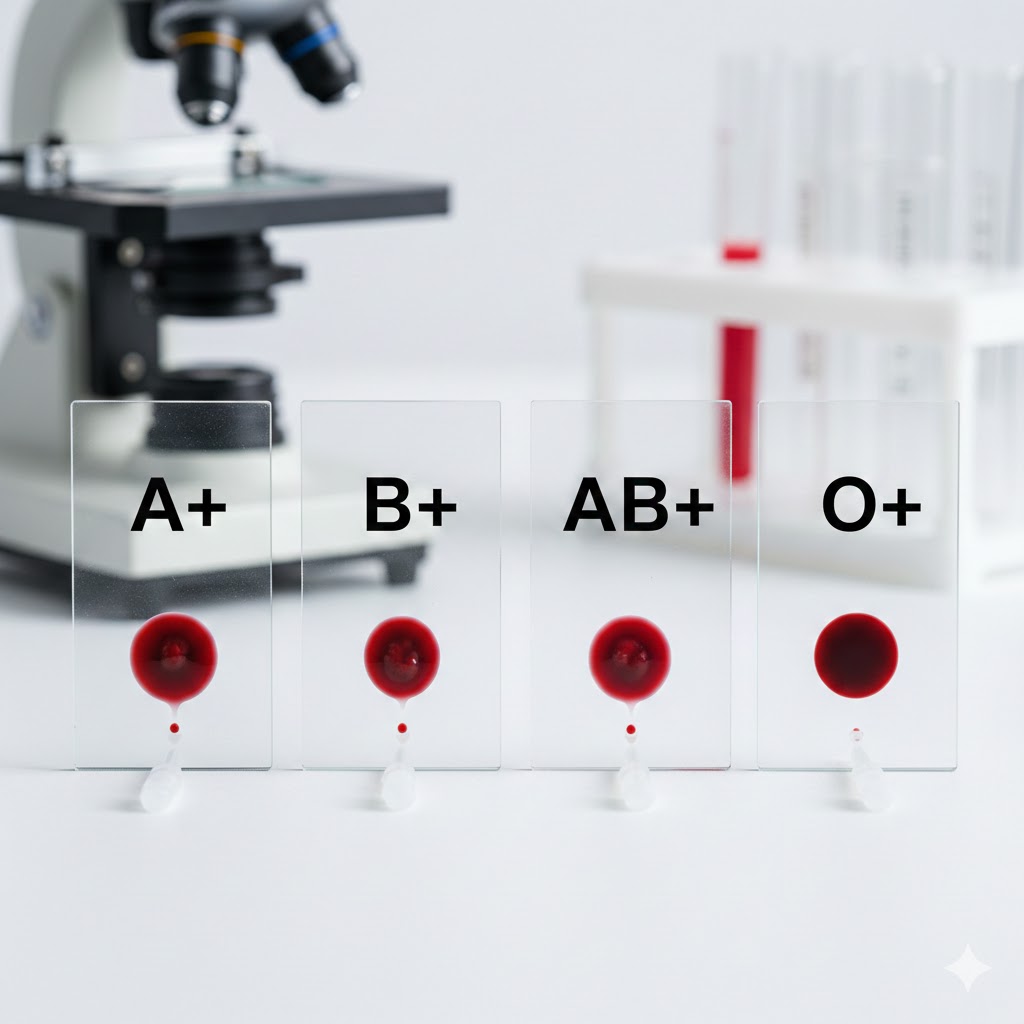
ABO AND Rh TYPING IS PERFORMED BY TWO METHOD:- 1.SLIDE METHOD:- Aim: – ABO grouping and Rh typing using the slide method. Objective: – ABO grouping and Rh typing using the slide method, which is a standard procedure for determining an individual’s ABO and Rh blood types. Principle: – ABO grouping and Rh typing performed by antisera based on the principle of agglutination. Normal human red cell processing antigen will clump in the presence of corresponding antibody (Anti A, Anti B, Anti D). Requirement:- *whole blood sample (EDTA) *Disposable gloves *Clean glass slide *ABO grouping and Rh typing reagents *Toothpicks or wooden sticks *Droppers of pipettes *Absorbent paper towels *Timer or stopwatch *Blood typing record sheet. Preparation:- Ensure that you are working in a well-lit and clean laboratory environment Label each glass slide with the patient’s identification or sample number Put on disposable gloves to maintain aseptic conditions ABO blood grouping procedure:-*Take three clean and dry glass slides *Place one drop of patient’s blood on each slide *Add a drop of Anti A reagent on first slide anti B on second slide, Anti D on third slide. *Mix the blood and serum gently using separate wooden sticks. Observation and record the reaction: – *if blood agglutinates (clumps)with anti A serum then the patient blood group is A. *If blood agglutinates with anti B serum, then the patient blood group is B. *If blood agglutinates with anti A and anti B both serums, then the blood group is AB. *If blood do not agglutinate with both anti A and anti B serum, then the blood group is O. Antisera A Antisera B Blood group + – A – + B + + AB – – O Rh blood grouping procedure: – Take clean and dry glass slide Place a fresh drop of the patient blood on slide Add a drop of anti Rh (anti D) serum. Mix gently with wooden stick. Observation and record the reactions: – if the blood agglutinates with anti Rh serum, then the patient blood Rh positive e.g. (A+, B+, AB+, O+) If blood is not agglutinate with anti Rh serum, then the patient blood Rh negative e.g. (A-, B-, AB-, O-) Antisera D Blood group + Rh positive – Rh negative Clinical significance: – ABO grouping and Rh typing is important in: – *.Blood transfusion *.Used for the personal identification and paternity exclusion (before DNA testing) *.Before a person donates blood. *.Before an organ and tissue transplant *.Before surgery *.To show whether to people could be blood relatives *.To check the identity of a person suspected of committing a crime. Note: – The ABO and Rh typing determination is used for the transfusion safety, pregnancy management, transplantation, forensic identification, and understanding disease susceptibility. TEST TUBE METHOD:- AIM: – ABO grouping and Rh typing by test tube method. Principle: –In the ABO grouping and Rh typing using the antisera is based on the principle of agglutination. Normal human red cell processing antigen will clump in the presence of corresponding antibody. Requirements: – blood group tube Pasteur pipettes. Centrifuge. Reagent. Normal saline. Blood sample. Procedure: – Prepare 5% red cell suspension for ABO grouping and Rh typing. Mix 5 drops(0.05ml) of sediment red cell with 2 ml of normal saline. Centrifuge at 1500 rpm for 1–2-minute discard the supernatant part wash 3 time with normal saline. Add 4ml of normal saline to sedimented red blood cells. Take 3 test tube label them as A, B, D. Place 1 drop of anti A into ‘A’ tube, one drop of anti B into the ‘B’ tube. one drop of anti D in ‘D’ tube. Add one drop of RBC suspension to each tube. Gently shake each tube to mix the contents. And then centrifuge tube at 1500 rpm for 1 minute. The RBC will form a button or pellet at the bottom of each test tube. Gently resuspend the RBC button and examine agglutination macro and microscopically. Observation: – Antisera A Antisera B Blood group + – A – + B + + AB – – O Antisera D Blood group + Rh positive – Rh negative