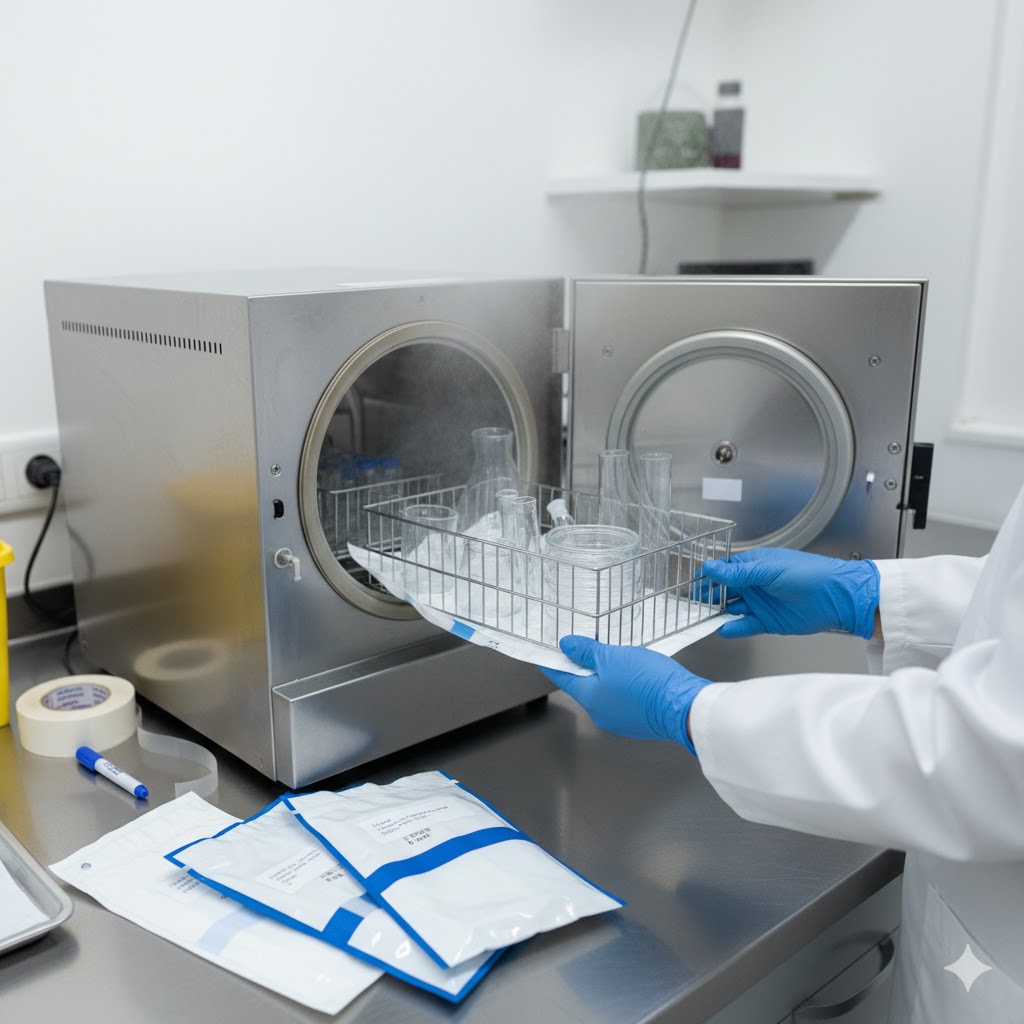
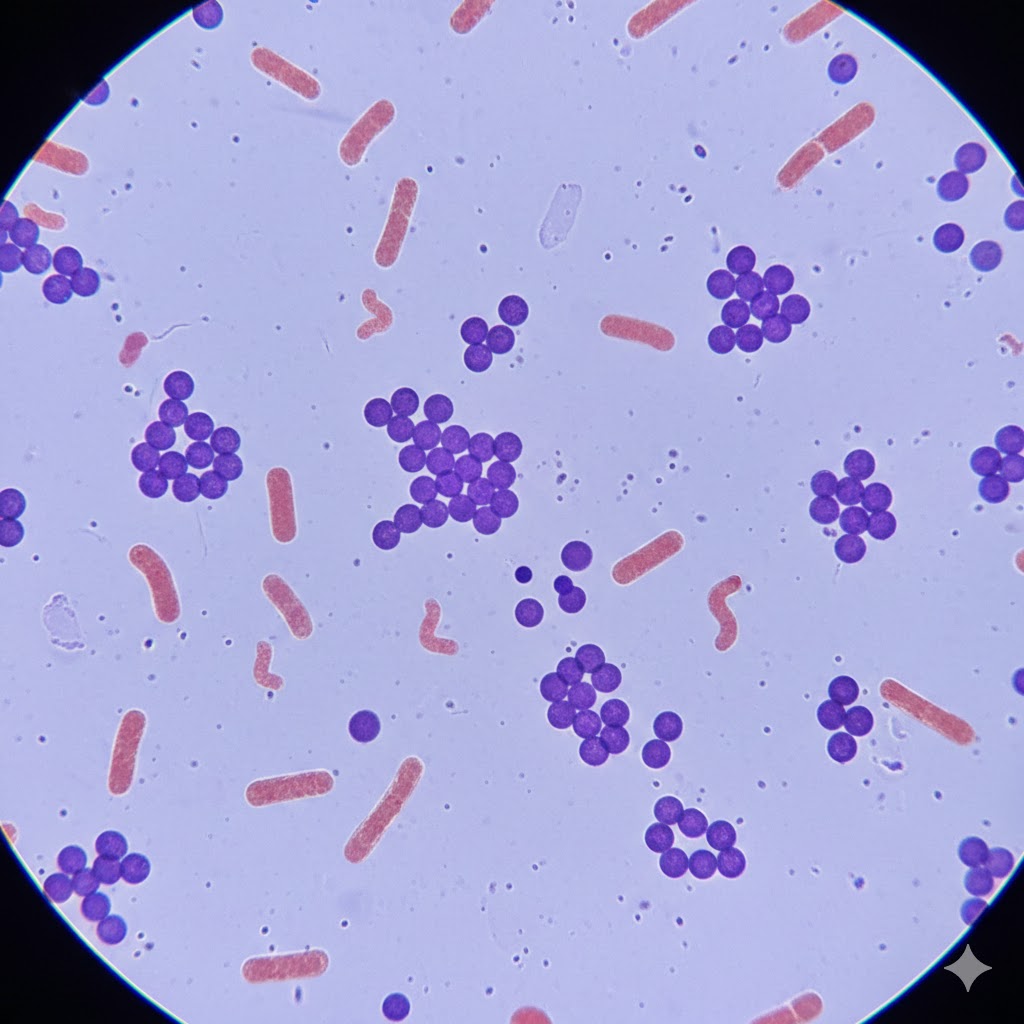
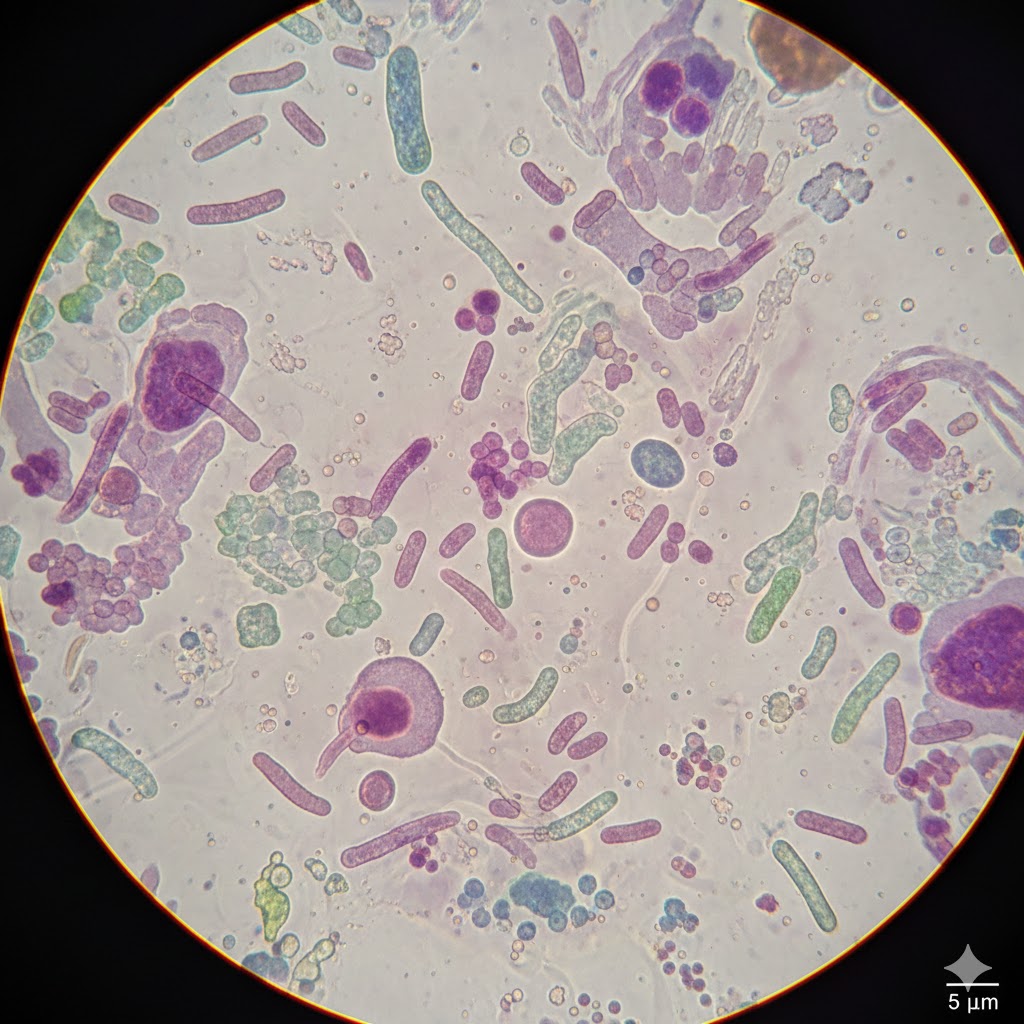
STERILIZATION:- Sterilization (or sterilisation) refers to any process that eliminates, removes, kills, or deactivates all forms of life and other biological agents.(suchas:- fungi, bacteria, viruses, spore forms, prions, unicellular eukaryotic organisms such as Plasmodium, etc) present in a specified region, such as a surface, a volume of fluid, medication, or in a compound such as biological culture media. Sterilization can be achieved through various means, including: heat, chemicals, irradiation, high pressure, and filtration. Sterilization is distinct from disinfection, sanitization, and pasteurization, in that sterilization kills, deactivates, or eliminates all forms of life and other biological agents which are present. Sterilization are classified as following:- physical methods of seterilization (i)Sun-Light:- Ultraviolet rays present in the sun-light are responsible for spontaneous sterilization in natural conditions. In tropical countries the sun light is more effective in killing bacteria due to combination of ultraviolet rays and heat. By killing bacteria in suspended water, sunlight provides natural method of disinfection of water bodies such as tanks and lakes. Those articles which cannot withstand high temperature can still be sterilised at lower temperature by prolonging the duration of exposure. (ii)Heat:- It is considered to be the most reliable method of sterilization of articles—that withstand heat. There are two methods of the sterilization: dry heat and moist heat. (A) Dry Heat: It acts by protein denaturation and oxidative damage. Sterilization by dry heat is as follows:- (a) Red Heat: Articles such as bacteriological loops, straight wires, tips of forceps and searing spatulas are sterilised by holding them in a Bunsen flame, till they become hot red. (b) Flaming: Articles are passed over a Bunsen flame but not heating it to redness. (c) Incineration: Contaminated, materials are destroyed by burning them in incinerator. (d) Hot Air Oven: Articles are exposed to high temperature (160°C) for duration of one hour in an electrically heated oven (method was introduced by Louis Pasteur). (B) Moist Heat: It acts by coagulation and denaturation of proteins. (i)At Temperature below 100°C: Pasteurization: This process was originally employed by Louis Pasteur. Currently this procedure is employed in food and dairy industry. There are two methods of pasteurization, the holder method (heated at 63oC for 30 minutes) and flash method (heated at 72oC for 15 seconds) followed by quickly cooling to 13oC. Other pasteurization methods include Ultra-High Temperature (UHT), 140oC for 15 sec and 149oC for 0.5 sec. This method is suitable to destroy most milk borne pathogens like Salmonella, Mycobacterium, Streptococci, Staphylococci and Brucella, however Coxiella may survive pasteurization. Efficacy is tested by phosphatase test and methylene blue test. Vaccine bath:- The contaminating bacteria in a vaccine preparation can be inactivated by heating in a water bath at 60oC for one hour. Only vegetative bacteria are killed and spores survive. Serum bath:- The contaminating bacteria in a serum preparation can be inactivated by heating in a water bath at 56oC for one hour on several successive days. Proteins in the serum will coagulate at higher temperature. Only vegetative bacteria are killed and spores survive. (ii) At Temperature 100°C:- (a)Boiling:- Boiling water (100C°) kills most vegetative bacteria. (b) Steam at 100°C:- Passing the steam at 100°C over articles kills bacteria. Sugars and gelatin in medium may get decomposed by autoclaving. So, these can be sterilised by exposing them to free steaming for 20 minutes for three successive days. This process is known as tyndallisation (after John Tyndall). (iii)At Temperature above 100°C:- (a) Autoclave:- Sterilization can be effectively achieved at a temperature above 100°C using an autoclave. Structure of Autoclave:- A simple autoclave has vertical or horizontal cylindrical body with a heating element, a per-forted tray to keep the articles, a lid that can be fastened by screw clamps, a pressure gauge, a safety valve and a discharge tap (Fig. 1). The lid is closed but the discharge tap is kept open and the water is heated. As the water starts boiling the steam drives air out of the discharge tap, when all the air is displaced and steam starts appearing through the discharge tap, the tap is closed. The pressure inside is allowed to rise up to 15 lbs. per square inch. At this pressure the articles are heated for 15 minutes, after which the heating is stopped and the autoclave is allowed to cool. Once the pressure gauge shows the pressure equal to atmospheric pressure, the discharged tap is opened to let the air in. The lidis opened and articles are removed. Culture media, dressing, certain equipment’s can be sterilised by autoclave. (iii) Sonic and Ultrasonic Vibrations- Sound waves of frequency 720,000 cycle/second kills bacteria and some viruses exposing for one hour. (iv) Radiation:- Two types of rays are used for sterilization: Non-ionizing and ionizing. (a) Non-Ionizing Rays:- These are low-energy rays with poor penetrative power, e.g., U.V. rays (wavelength 200-280 nms, effective 260 nm). (b) Ionizing Rays:- These are high-energy rays with good penetration power. These are of two types:- Particulate and electromagnetic.Electron beams are particulate while gamma rays are electromagnetic in nature. High speed electrons are produced by a linear accelerator from a heated cathode. Electromagnetic rays such as gamma rays emanate from nuclear disintegration of certain radioactive isotopes (Co60, Cs137). A degree of 2.5 megabrands of electromagnetic rays kills all bacteria, fungi, virus and spores. In some parts of Europe, fruits and vegetable are irradiated to increase their shelf life up to 500 percent. Since radiation does not generate heat, it is called Cold sterilization. Chemical Methods of Sterilization: Chemicals destroy pathogenic bacteria from inanimate surfaces and are all also called disinfectants. Liquid:- Alcohols:- E.g., Ethyl alcohol, Isopropyl alcohol and methyl alcohol. (A 70% solution kills bacteria). Aldehydeles: E.g.,Fomaldehyele,Gluteraldehydele(40% formaldehyde is used for surface disinfection). Phenol:- E.g., 50% phenol, 1-5% cresol, 5% lysol, chloroxylenol (Dettol). Halogens: E.g.,chlorine compounds (chlorine bleach, hydrochloride) and iodine compounds (tincture, iodine, iodophores). Tincture of iodine (2% iodine in 70% alcohol) is antiseptic. Heavy metals:- E.g., Mercuric chloride, silver nitrate, copper sulfate, organic mercuric salts. Surface active agents: e.g., soaps or detergents. Dyes:- Acridin dyes e.g., acriflavin and aminacrine are bactericidal (interact with bacterial nucleic acids). Gaseous: E.g.Ethylene oxide, formaldehyde gas, highly effective, killing of spores. Physiochemical Methods of Sterilization: A